BLOOD BRAIN BARRIER PERMEABILITY, INFLAMMATION AND INTESTINAL PERMEABILITY IN AUTISM
A recent article published in Molecular Autism has offered some controversial suggestions that the blood brain barrier in autism is disrupted and that this may be somehow related to gastrointestinal symptoms. The article, whose lead author was Maria Fiorentino, was entitled, “Blood-brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders”. This study analyzed postmortem samples of the cerebral cortex and cerebellum from 33 individuals (8 of them with autism) and found altered expression of genes related to blood-brain barrier integrity and inflammation. The group then analyzed gastrointestinal tissue from a different cohort having 12 individuals with ASD and 9 controls. The analysis showed that a majority of ASD individuals had reduced expression of “barrier forming cellular components” and a higher expression of molecules associated with increased intestinal permeability. From the results the authors drew a correlation between brain and gastrointestinal permeability. As for future research Dr. Fiorentino will study how the bacteria of the gut is related to intestinal permeability and behavioral symptoms.
The article is an example of that old saying: “When you have a hammer everything looks like a nail”. Indeed, the authors performed a study with inappropriate techniques to reach a conclusion that they were pursuing beforehand- and found it. The major weakness of the study is not having anybody on their team that actually knew about the blood-brain barrier and the different confounds of working with postmortem tissue.
Inflammatory reactions and disruption of the blood brain barrier provide fingerprints that can be examined by the pathology laboratory. As an example, consider the cerebrospinal fluid (CSF). This is the liquid that bathes the brain and spinal cord. It is produced within a cavernous entity in the brain called the ventricles. The CSF is the end result of a highly filtrated liquid originating from capillaries that protrude in finger-like projections of tissue into the ventricles. The tissue with the protrusions is called the choroid plexus. The CSF liquid is very diluted and contains a very reduced concentration of proteins as compared to blood. Whenever the blood-brain barrier is disrupted more protein from the blood is able to transverse the barrier thus increasing its concentration. Occasionally the disruption is so big that even blood cells will cross the barrier.
During inflammation, in addition to increasing the concentration of proteins, the types of protein are also changed. Under normal conditions the brain does not allow certain types of proteins, usually the larger ones, to transverse the blood vessel walls (thus the name blood-brain barrier). Albumin is the most abundant protein in human blood. It is a large molecule usually made bigger by transporting other molecules like hormones and fatty acids. It is produced in the liver and is never found in the normal human brain. The same can be said for immunoglobulins. A lot of research from Pharmaceutical industries has been focused on disrupting the blood brain barrier in order to let immunoglobulins (antibodies) to the brain. Thus far numerous studies have been done showing normal protein concentrations and no evidence of albumin or immunoglobulins in the brains of ASD individuals.
In addition to studies of the CSF’s composition, disruption of the blood-brain barrier/edema and inflammation can be studied under the microscope. Edema is mostly seen as excess accumulation of fluid within the brain. If it is a major accumulation of fluid, the brain becomes bigger, softer and the ridges of the cerebral cortex surrounding the brain become flattened. Under the microscope the background of the brain looks frazzled and the liquid extruded from the blood vessels expand the periventricular spaces (see figures below). Although hundreds of brains have been thoroughly investigated, including some using serial sections of whole brains examined from front to back. If changes were present, they would have been found.
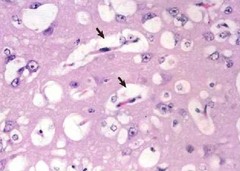
Figure: Section of the white matter with prominent spaces around the blood vessels (arrows). The figure portrays edema caused by rupture of the blood-brain barrier.

Figure: White matter of a control individual (left) and that of an edematous brain (right). The frazzled appearance of the brain is evident when disruption of the blood-brain barrier causes edema. This is not typical of the brains of autistic individuals.
The Fiorentino study took the lazy approach of using inappropriate techniques- which were apparently the only ones known to the researchers. They also studied indirect measures based on gene expression that suffered the same confounds as other postmortem studies. Basically, brains of ASD individuals differ from neurotypicals as to mode of death and preagonal conditions. This alone could have accounted for their findings. A defect of the blood brain barrier would probably cause chronic deterioration of the brain. This is not what happens in autism. Let’s review the literature and use common sense before designing our studies. It is a pity that articles like the one discussed appear in the literature and only serve to confuse the real findings and steer research in inappropriate directions.
References
Fiorentino M, Sapone A, Senger S, Camhi AA, Kadzielski SM, Buie TM, Kelly DL, Cascella N, Fasano A. Blood-brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders. Molecular Autism, 2016; 7(1) DOI 10.1186/s13229-016-0110-z
Hiç yorum yok:
Yorum Gönder